The decision to treat a varicocele is often based on the severity of symptoms, the potential impact on fertility, and other individual factors.
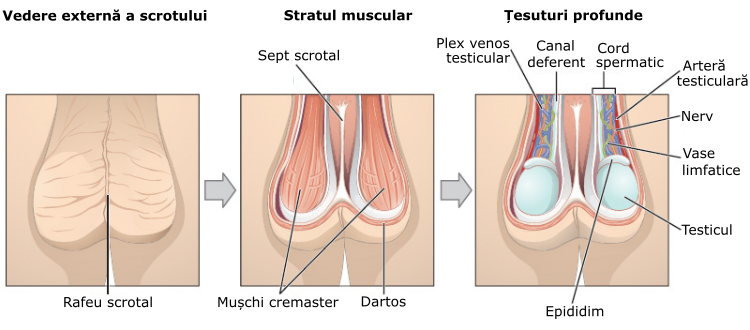
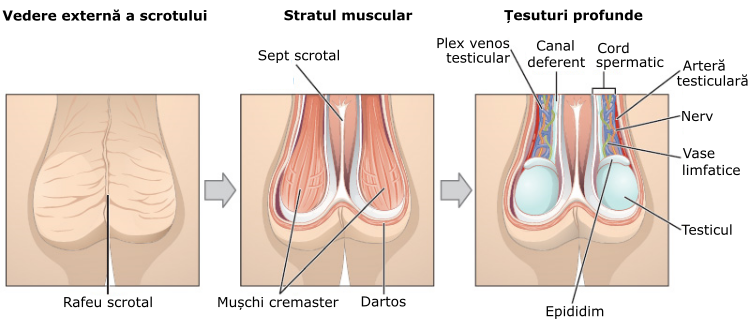
A varicocele is a medical condition characterized by the enlargement of the veins within the scrotum, which is the pouch of skin containing the testicles. These veins are called the pampiniform plexus, and they can become dilated and swollen, similar to varicose veins that occur in the legs. Varicoceles are most commonly found on the left side of the scrotum.
The exact cause of varicoceles is not always clear, but it is often associated with the malfunction of the valves within the veins, leading to a backflow of blood and resulting in the enlargement of the veins. Varicoceles are more commonly observed in males aged 15 to 25.
While some varicoceles may cause no symptoms, others can be associated with discomfort, pain, or swelling in the scrotum. Varicoceles are also known to be a common cause of male infertility. Increased blood flow and elevated temperatures around the testicles due to varicoceles may affect sperm production and quality.
Causes
The exact cause of varicoceles is not always clear, but the condition is thought to result from problems with the valves within the veins that regulate blood flow.
When these valves fail to function properly, blood can pool in the veins, causing them to enlarge and become varicose. Several factors may contribute to the development of varicoceles:
- Faulty Valves: The primary cause is often attributed to malfunctioning valves in the veins of the spermatic cord. These valves normally prevent blood from flowing backward, but if they fail, blood accumulates, leading to vein enlargement.
- Anatomy: Some individuals may have natural variations in their anatomy that make them more prone to developing varicoceles.
- Blood Flow Obstruction: Conditions that lead to increased pressure within the abdomen, such as a tumor or other mass, can obstruct blood flow and contribute to the development of varicoceles.
- Genetics: There might be a genetic component, as varicoceles tend to run in families. If close relatives have had varicoceles, an individual may be at a higher risk of developing them.
Symptoms
The symptoms of a varicocele can vary, and some individuals may not experience any noticeable signs. Common symptoms may include:
- Visible or Palpable Swelling: Often described as feeling like a bag of worms, the veins in the scrotum may be visibly enlarged or felt through the scrotal skin.
- Scrotal Discomfort or Pain: Individuals with varicoceles may experience a dull, aching pain or discomfort in the scrotum. This discomfort might increase with physical exertion or prolonged periods of standing.
- Testicular Atrophy (Shrinkage): In some cases, a varicocele may lead to the shrinking of the affected testicle, although this is more commonly associated with larger or more severe varicoceles.
- Fertility Issues: Varicoceles are a known cause of male infertility. They can affect sperm quality and production due to increased blood flow and elevated temperatures in the testicles.
It’s important to note that not everyone with a varicocele experiences symptoms, and the condition is sometimes discovered during a routine physical examination or fertility testing.
Diagnosis
Diagnosing a varicocele typically involves a combination of medical history review, physical examination, and sometimes imaging studies. Here’s how healthcare professionals may test for a varicocele:
- Medical History:
- The healthcare provider will begin by asking about the patient’s symptoms, including any pain or discomfort in the scrotum, changes in testicle size, and fertility concerns. Providing information about the onset and duration of symptoms is important for diagnosis.
- Physical Examination:
- During a physical examination, the healthcare provider may ask the patient to stand and perform a Valsalva maneuver, which involves bearing down as if having a bowel movement. This helps in assessing any changes in the size of the veins within the scrotum. The healthcare provider will feel the scrotum for any abnormalities, such as swelling or a mass.
- Scrotal Ultrasound:
- If a varicocele is suspected or if there are concerns about fertility, a scrotal ultrasound may be performed. This imaging test uses sound waves to create a detailed image of the veins in the scrotum. It can help confirm the presence of a varicocele, assess its size, and rule out other potential causes of scrotal swelling.
- Doppler Ultrasound:
- A Doppler ultrasound, which measures blood flow through the veins, can be particularly useful in diagnosing varicoceles. It provides information about blood flow patterns and can help differentiate varicoceles from other conditions.
It’s essential to note that not all varicoceles cause symptoms, and the decision to treat a varicocele depends on factors such as the severity of symptoms, the impact on fertility, and the patient’s overall health.
Treatment
Treatment options range from conservative measures to more invasive procedures. Here are common approaches:
- Observation (Conservative Management):
- Not all varicoceles require active treatment, especially if they are asymptomatic and not causing fertility issues. In such cases, the healthcare provider may recommend observation, monitoring the condition over time to ensure it does not worsen.
- Scrotal Support:
- Wearing supportive underwear or a scrotal support device (like a jockstrap) can help alleviate discomfort associated with a varicocele by reducing pressure on the veins.
- Pain Management:
- Over-the-counter pain relievers, such as ibuprofen or acetaminophen, may be recommended to manage pain or discomfort.
- Fertility Treatments:
- In cases where a varicocele is associated with male infertility, treatment options may focus on improving fertility. Surgical correction of the varicocele (varicocelectomy) is a common approach in such situations.
- Embolization:
- Varicocele embolization is a minimally invasive procedure where a catheter is used to block the abnormal veins, redirecting blood flow and reducing the size of the varicocele. This procedure is often performed by an interventional radiologist.
- Surgical Varicocelectomy:
- This surgical procedure involves ligating (tying off) the dilated veins to redirect blood flow and reduce the size of the varicocele. It can be performed through an open surgical approach or using minimally invasive techniques such as laparoscopy or microsurgery.
Varicocelectomy is often considered when there is pain, testicular atrophy, or concerns about fertility. However, not all varicoceles require intervention, and conservative measures may be sufficient for those without significant symptoms or fertility issues.
Prognosis
The prognosis for individuals with a varicocele is generally favorable, especially when the condition is asymptomatic or only mildly symptomatic. Varicoceles are a common and treatable cause of male infertility, and interventions such as varicocelectomy can improve fertility outcomes in some cases. However, the prognosis can vary based on several factors:
- Severity of Symptoms: Asymptomatic or mildly symptomatic varicoceles may not significantly impact a person’s quality of life. Conservative measures, such as scrotal support, pain management, or observation, may be sufficient in such cases.
- Fertility Concerns: For individuals experiencing male infertility associated with a varicocele, the prognosis may be improved through fertility treatments, including varicocelectomy. However, it’s important to note that not all cases of male infertility are related to varicoceles, and individual fertility factors can vary.
- Treatment Approach: The choice of treatment can influence the prognosis. Surgical interventions like varicocelectomy or minimally invasive procedures such as embolization have been shown to be effective in improving sperm parameters and fertility outcomes in some cases.
- Underlying Causes: In cases where varicoceles are secondary to an underlying condition, such as obstruction of the spermatic vein or other vascular abnormalities, addressing the root cause may be necessary for a more favorable outcome.
- Complications: While uncommon, complications from varicocele treatment, such as recurrence, hydrocele formation (fluid accumulation in the scrotum), or infection, can affect the overall prognosis. These complications are typically rare when procedures are performed by experienced healthcare professionals.
Conclusion
It’s crucial for individuals with varicoceles to consult with a urologist or a healthcare professional specializing in reproductive health to determine the most appropriate course of action based on their specific circumstances. Regular follow-up appointments may be recommended to monitor any changes in symptoms or fertility status.
It’s important to note that the presence of a varicocele does not guarantee fertility issues, and not all individuals with varicoceles will require treatment.
Each case is unique, and the prognosis is best discussed with a healthcare professional who can provide personalized guidance based on the individual’s health, symptoms, and fertility concerns.